Sickle Cell Disease
- 18 Nov 2025
In News:
Recent medical findings from a decade-long study conducted at Fortis Memorial Research Institute (FMRI), Gurugram, have demonstrated significant success in curing Sickle Cell Disease (SCD) in children through bone marrow (stem cell) transplantation. The study, published in the journal Haemoglobin,analysed100 paediatric cases treated between 2015–2024, reporting an overall survival rate of 87%, with 96% success in matched sibling donor transplants and 78% success in half-matched (haploidentical) family donor transplants. These outcomes place India among the leading countries in advanced paediatric transplant care, particularly notable because SCD disproportionately affects India and sub-Saharan Africa, which together account for nearly half of global cases.
About Sickle Cell Disease
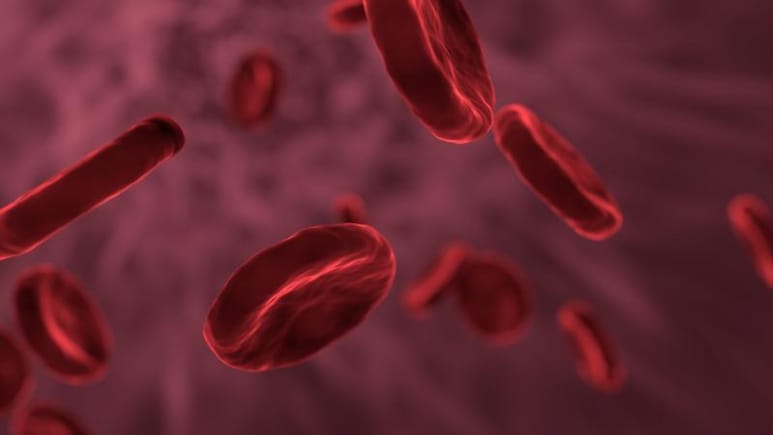
Sickle Cell Disease is a genetic blood disorder caused by the inheritance of two defective genes encoding hemoglobin S—one from each parent. It affects hemoglobin’s structure and function. Normally, red blood cells (RBCs) are round, flexible, and able to move smoothly through blood vessels. In SCD, RBCs distort into a sickle or crescent shape, become rigid and sticky, and obstruct blood flow. This blockage reduces oxygen delivery to tissues and leads to severe pain episodes, organ damage, stroke risk, and a shortened lifespan. The most severe form is Sickle Cell Anemia.
Symptoms
- Early childhood: Persistent tiredness, anemia, painful swelling of hands and feet, jaundice
- Later stages: Recurrent pain crises, infections, stroke, liver and kidney damage, chronic anemia
Causes
- Inherited autosomal recessive disorder
- A child must inherit two copies of the defective sickle cell gene
- Carriers (with one defective gene) do not have the disease but may pass it on
Treatment Approaches
1. Bone Marrow (Stem Cell) Transplant
- Currently the only curative treatment for SCD
- Involves replacing defective bone marrow with healthy stem cells
- FMRI study shows high success rates, comparable to global standards
- Early diagnosis and timely transplant significantly improve survival
2. Supportive Medical Care
- Pain management
- Blood transfusions
- Infection control
- Prevention of complications
3. Gene Therapy (Emerging)
- UK became the first country to approve a gene therapy cure
- Targets and corrects the defective gene producing hemoglobin S
Significance of India’s Transplant Success
The FMRI study demonstrates that developing countries can achieve outcomes similar to the most advanced clinical centres worldwide when equipped with appropriate medical infrastructure and protocols. The success is attributed to:
- Use of reduced-toxicity conditioning regimens
- Adoption of post-transplant cyclophosphamide (PTCy) to reduce graft-versus-host disease (GVHD)
- Expansion of haploidentical (half-matched) donor options when full sibling matches are unavailable
- Strengthened donor registries, early diagnosis, and improved infection control
The findings indicate that cost-effective and safe transplant strategies can be scaled in India and Africa, improving access for children in low-resource settings.
Public Health Relevance
Sickle Cell Disease is a major public health challenge in India, especially among tribal populations in central and western India. Improving outcomes requires:
- Early screening
- Increased awareness
- Strengthening transplant facilities
- Improved donor availability
- Supportive state and national programs
The success of bone marrow transplantation offers a model for scalable, curative intervention for millions living with SCD, demonstrating India’s growing capability in advanced paediatric care.
Govt Mulling Incentives for ASHA Workers (ET)

- 09 Oct 2023
Why in the News?
The government is planning to give incentives to ASHA health activists for mobilising eligible individuals for sickle cell disease screening and distribution of sickle cell cards for prevention and early detection of the disease.
About Accredited Social Health Activist (ASHA):
- ASHA serves as a trained female community health activist integral to the National Rural Health Mission initiated by the Government of India.
- Selected from the community and accountable to it, ASHA is trained to bridge the gap between the community and the public health system.
Key Functions:
- Acts as a care provider at the community level.
- Facilitates access to healthcare, medicine, and sanitation services.
- Health Awareness: Raises awareness of health issues among marginalized sections within the community.
- Advocate for Women's Health: Champions female health and hygiene standards.
- Advocates for a health-conscious approach to livelihood.
Implementation:
- The ASHA scheme is operational in all States/UTs, except Goa.
- States are mandated to employ at least one ASHA worker per every 1000 people.
- Inclusive Selection Process: The selection process involves various community groups, self-help groups, Anganwadi Institutions, and local committees.
Selection Criteria:
- Rural ASHA: Preferably a literate woman resident, married/widowed/divorced, aged 25 to 45 years, and preferably educated up to the 10th standard.
- Urban ASHA: Identified from vulnerable clusters, belonging to specific vulnerable groups, with good communication and leadership skills.
Compensation:
- Primarily an honorary volunteer compensated for specific situations.
- Ranges from Rs 2,000 to Rs 7,000, depending on the state.
- Incentives: Eligible for incentives under various national health programs.
