Step-and-Shoot Spot-Scanning Proton Arc Therapy (SPArc)
- 15 Jun 2025
In News:
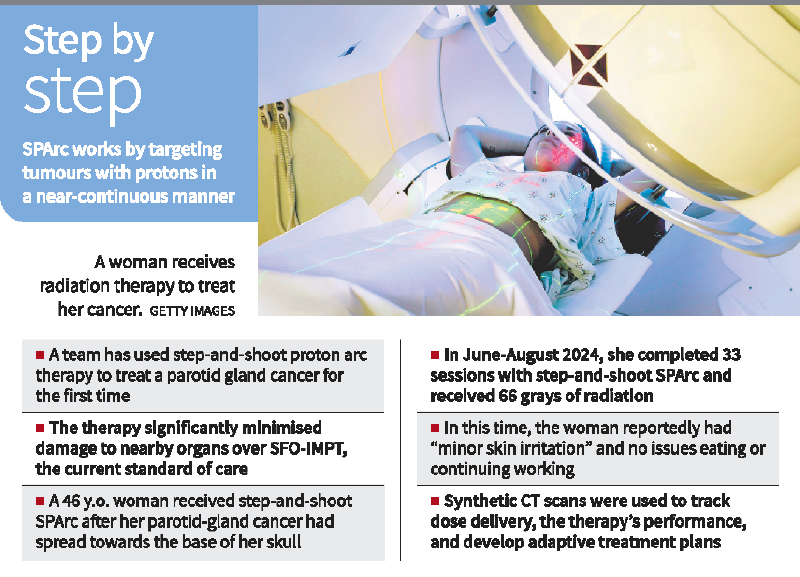
In a significant medical advancement, a team at the Corewell Health William Beaumont University Hospital in the U.S. has successfully administered Step-and-Shoot Spot-Scanning Proton Arc Therapy (SPArc) to treat adenoid cystic carcinoma—a cancer originating in the parotid gland. This marked the first-ever clinical application of this technology. The findings were published in the International Journal of Particle Therapy in June 2025.
What is SPArc Therapy?
SPArc (Spot-Scanning Proton Arc Therapy) is an advanced form of proton beam therapy where proton particles are delivered in a controlled arc across the tumor. It includes two primary modalities:
- Step-and-Shoot SPArc: Follows a pre-programmed dose delivery path.
- Dynamic SPArc: Simulated version where energy levels and targeting points are adjusted in real-time. (Still under regulatory review)
Comparison with Existing Techniques
The study compared three techniques:
- SFO-IMPT (Single-Field Optimized Intensity-Modulated Proton Therapy – current standard)
- Step-and-Shoot SPArc (clinical)
- Dynamic SPArc (simulated)
SPArc showed reduced radiation exposure to key organs when compared with SFO-IMPT:
- Brainstem: ↓ 10%
- Optical chiasm: ↓ 56%
- Oral cavity: ↓ 72%
- Spinal canal: ↓ 90%
Treatment Case Study
The first patient treated was a 46-year-old woman with a tumor extending from her parotid gland to the base of her skull. She underwent 33 sessions of SPArc therapy from June to August 2024, reporting only minor skin irritation and no disruptions to eating or daily functioning.
Process & Technology Used:
- Cone-Beam CT (CBCT) was used for real-time imaging before each session.
- A machine learning model converted CBCT to synthetic CT, allowing accurate dose tracking.
- As the patient lost weight, the dose plan was adjusted after two weeks to maintain precision.
- Nine beam angles spanning a 180º arc were used, delivering radiation at 20º intervals.
Each session lasted about 15–18 minutes, enabling nearly continuous dose delivery.
Working Mechanism
- The therapy operates by 'painting' the tumor in energy layers.
- Each energy level targets a specific tissue depth, ensuring maximum precision.
- The system scans dozens of spots in each layer before moving to the next one with increased penetration.
Advantages
- High precision in delivering radiation to deep and complex anatomical regions like the skull base.
- Limits collateral damage to vital organs.
- Effective in large or invasive tumours.
- Better quality of life during treatment (reduced side effects such as fatigue or swallowing issues).
Limitations & Concerns
- Geographical miss risk: Tiny tumors may be missed due to breathing motion or tumor shrinkage over time.
- Cost: High installation and operational costs, making it suitable for a limited patient base.
- Potential for overuse in non-indicated cases, leading to inequitable healthcare delivery.
- Dynamic SPArc still awaits regulatory clearance and integration into oncology systems.
Significance for India
SPArc therapy can be transformative for cancers in anatomically intricate regions and may serve as a benchmark for future precision cancer therapies. However, adoption in India requires cost-reduction, infrastructure investment, and regulatory frameworks.
