WHO Pandemic Agreement: A Landmark Step Towards Global Health Security

- 21 May 2025
Context:
The World Health Assembly (WHA), the decision-making body of the World Health Organization (WHO), adopted the first-ever Pandemic Agreement at its 78th session in May 2025. This historic and legally binding agreement, three years in the making, aims to strengthen global pandemic preparedness, prevention, and response with a focus on equity, solidarity, and scientific evidence. Triggered by the gaps and inequities exposed during the COVID-19 crisis, the accord marks a milestone in global health governance under Article 19 of the WHO Constitution, previously used for the 2003 Framework Convention on Tobacco Control.
The agreement was unanimously approved by 124 countries, with no opposition and 11 abstentions. It emphasizes that national sovereignty remains intact, explicitly stating that WHO cannot mandate domestic laws or measures such as lockdowns, vaccine mandates, or travel restrictions. This provision addresses concerns of state overreach and promotes voluntary, collaborative international action.
A central feature is the creation of a Pathogen Access and Benefit Sharing (PABS) system, wherein countries that share virus samples will receive equitable access to vaccines, diagnostics, and therapeutics. Participating pharmaceutical companies must allocate 20% of their real-time production (10% as donations, 10% at affordable prices) to WHO for distribution based on public health needs, especially in developing nations. This move addresses the vaccine nationalism witnessed during COVID-19 and promotes global health equity.
To support this system, the agreement calls for the establishment of a Global Supply Chain and Logistics Network (GSCL), coordinated by WHO, to ensure timely and fair distribution of essential health products during public health emergencies. Member states are encouraged to develop national pandemic prevention plans, improve disease surveillance, and invest in routine immunisation, antimicrobial resistance control, and zoonotic disease prevention.
Another key pillar is the promotion of sustainable local production of health products and technology transfer to developing countries. Mechanisms such as licensing, regulatory incentives, and financing are to be used to facilitate regional and global tech hubs. These efforts are aimed at reducing reliance on a few manufacturing nations and improving rapid response capabilities globally.
The agreement’s adoption is politically significant in reaffirming multilateralism amid rising nationalism. WHO Director-General Dr. Tedros Adhanom Ghebreyesus hailed it as a “victory for public health and multilateral cooperation.” However, the absence of the United States — a major global health funder and former leader in pandemic response — casts a shadow. The U.S. withdrew from the drafting process following the Trump administration’s move to exit WHO, raising concerns about the treaty’s universality and enforcement.
Despite the lack of a penalty mechanism for non-compliance, the agreement represents a global consensus on shared responsibility for health security. It acknowledges that pandemics pose transboundary risks requiring coordinated international action, especially to protect vulnerable populations and frontline workers.
Expected to enter into force after ratification by 60 countries and the finalisation of PABS and GSCL mechanisms by May 2026, the WHO Pandemic Agreement is a pivotal step in ensuring the world is better prepared, more resilient, and more just in the face of future pandemic threats.
WHO prequalifies a second malaria vaccine, a significant milestone in preventing the disease (WHO)
- 22 Dec 2023
Why is it in the News?
The World Health Organization (WHO) on Thursday added the R21/Matrix-M malaria vaccine, developed by Oxford University and manufactured by Serum Institute of India, to its list of prequalified vaccines.
News Summary:
- The R21/Matrix-M malaria vaccine, developed by Oxford University and produced by the Serum Institute of India, has received prequalification from the World Health Organization (WHO), marking a significant step in global efforts to combat malaria.
- This achievement follows the prequalification of the RTS, S/AS01 vaccine in July 2022, making R21 the second malaria vaccine to gain the WHO's approval.
- Prequalification means larger access to vaccines as a key tool to prevent malaria in children.
- The WHO employs rigorous international standards during the prequalification process, conducting a comprehensive evaluation to ensure the safety, efficacy, and adherence to global manufacturing standards of the vaccines.
- Ongoing measures, such as regular re-evaluation, site inspections, and targeted testing, are implemented to uphold prequalified vaccines’ continued safety and effectiveness.
What is a Prequalified Vaccine?
- The World Health Organization (WHO) defines a prequalified vaccine as one that has successfully completed a comprehensive three-step process prior to approval.
- Thorough Data Evaluation: The first step involves a meticulous examination of relevant data associated with the vaccine.
- Sample Testing: The second step includes rigorous testing of vaccine samples.
- Manufacturing Site Inspection: The final step encompasses an inspection of the pertinent manufacturing sites by WHO.
- Only when the outcomes of these steps are positive does the vaccine earn inclusion in the WHO list of Prequalified Vaccines?
What is Malaria?
- Malaria is an infectious disease caused by the Plasmodium parasite, transmitted to humans through the bites of infected female Anopheles mosquitoes, which are active mainly during the night.
- While there are numerous types of Plasmodium parasites, only five affect humans and cause malaria.
- Plasmodium falciparum: Predominantly found in Africa, it is the most common and lethal malaria parasite globally, responsible for the majority of malaria-related deaths.
- Plasmodium vivax: Primarily found in Asia and South America, this parasite causes milder symptoms than Plasmodium falciparum but can persist in the liver for up to three years, leading to potential relapses.
- Plasmodium ovale: Relatively uncommon and typically found in West Africa, this parasite can remain dormant in the liver for several years without causing symptoms.
- Plasmodium malariae: Rare and primarily found in Africa.
- Plasmodium knowlesi: Extremely rare and identified in certain parts of Southeast Asia.
Malaria Transmission:
- Upon being bitten by an infected mosquito, the Plasmodium parasite enters the bloodstream, travels to the liver, and matures.
- It then re-enters the bloodstream, invading red blood cells where it undergoes multiplication.
- Periodically, infected blood cells burst, releasing more parasites into the bloodstream.
- While mosquitoes can become infected by biting an already infected person, malaria does not spread directly from person to person.
Symptoms of Malaria:
- The signs and symptoms of malaria encompass fever, chills, general discomfort, headache, nausea, vomiting, diarrhoea, abdominal pain, muscle or joint pain, fatigue, rapid breathing, rapid heart rate, and cough.
- Recognizing these symptoms is crucial for prompt diagnosis and treatment.
What is the Status of Malaria in India?
- Given its predominantly tropical climate, a significant portion of India has a historical prevalence of malaria, and the country holds the distinction of being where Nobel Prize winner Sir Ronald Ross discovered the malaria parasite cycle involving Anopheles mosquitoes as the definitive host.
- While India has made substantial progress in the direction of malaria elimination, there remains a considerable journey ahead.
- According to the World Malaria Report 2023, India contributed to 66% of malaria cases within the World Health Organization’s South-East Asia region in 2022.
- Additionally, India and Indonesia jointly accounted for approximately 94% of all malaria-related deaths in the region last year.
- The report highlighted that nearly 46% of all cases in the region were attributed to Plasmodium vivax, a protozoal parasite and human pathogen.
What are the Challenges in Malaria Elimination?
- Eliminating malaria in India faces several challenges, primarily stemming from the predominant engagement of the private sector in diagnosing and treating the disease.
- This sector often encounters issues related to misdiagnosis and mistreatment.
Key challenges include:
- Limited Regulation in the Private Sector: Private doctors and clinics operate without an obligation to adhere to government guidelines, utilize recommended drugs, or report malaria cases to state authorities.
- Disproportionate Malaria Treatments in the Private Sector: In 2015, a substantial 86 million malaria treatments were procured in the private sector, in stark contrast to the meagre 2 million in the public sector.
- Proliferation of Artemisinin Monotherapy: The private sector annually acquires nearly 10 million injections of Artemisinin Monotherapy, a treatment strongly discouraged in India and globally due to its role in accelerating the development of lethal drug resistance.
- Irony of Drug Misuse: Remarkably, India, the largest supplier of high-quality approved malaria drugs globally, grapples with the ironic misuse of malaria drugs within its own borders.
Challenges in Creating a Malaria Vaccine:
The progress toward developing a malaria vaccine encounters various impediments:
- Absence of a Conventional Market: The absence of a conventional market poses a significant hindrance to the development of a malaria vaccine.
- Limited Developer Engagement: The involvement of only a few developers further complicates the landscape for malaria vaccine development.
- Technical Complexity: The technical intricacies associated with creating a vaccine against a parasitic infection, such as malaria, present substantial challenges.
- Complexity of Malaria Parasites' Life Cycle: Malaria parasites exhibit a complex life cycle, and there exists a limited understanding of the intricate immune response to malaria infection.
- Genetic Complexity of Malaria Parasites: The genetic complexity of malaria parasites, generating thousands of potential antigens, adds an additional layer of difficulty to the development of an effective vaccine.
Initiatives Taken by India for Malaria Eradication:
- Since 2000, India has successfully reduced malaria cases by more than half and malaria-related deaths by over 66%.
- In 2016, the country introduced its inaugural National Framework for Malaria Elimination (2016-2030), outlining a vision for a malaria-free nation by 2027 with complete elimination targeted by 2030.
- In 2019, the Government of India demonstrated its commitment by increasing funding for the National Vector Borne Disease Control Programme by over 25%.
- Furthermore, India augmented its support as a donor to the Global Fund to Fight AIDS, Tuberculosis, and Malaria, reaffirming its dedication to combating these vector-borne diseases on a global scale.
India Has the Highest Cases Of TB in The World: Global TB Report 2023 (NDTV)
- 09 Nov 2023
Why is it in the News?
According to the Global TB Report 2023 by the World Health Organisation, India had the highest number of Tuberculosis (TB) cases in the world in 2022.
What is the Global Tuberculosis Report?
- The Global Tuberculosis Report published by the World Health Organisation (WHO).
- It provides a comprehensive and up-to-date assessment of the TB epidemic and progress in prevention, diagnosis, and treatment of the disease at global, regional, and country levels.
- This is done in the context of global TB commitments, strategies, and targets.
- This report is based primarily on data gathered by WHO from national ministries of health in annual rounds of data collection.
Key Findings of the Global Tuberculosis Report 2023?
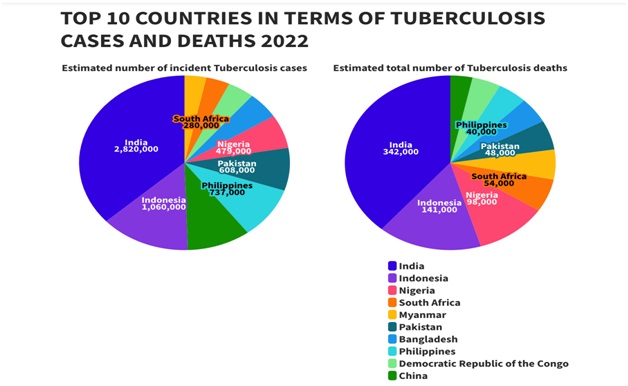
- India had the highest number of Tuberculosis (TB) cases in the world in 2022.
- The country accounted for 27 percent of the total TB cases in the world.
- The report revealed that 30 nations accounted for 87 percent of the world's TB cases.
- India was followed by Indonesia (10 per cent), China (7.1 per cent), the Philippines (7.0 per cent), Pakistan (5.7 per cent), Nigeria (4.5 per cent), Bangladesh (3.6 per cent), and the Democratic Republic of Congo (3.0 per cent).
- In the Case of the Fatality Ratio (the measure of how severe a disease is), India stood at 12 percent, which means 12 out of 100 patients died of the disease.
- Singapore had the lowest score of 1 percent while China stood at the 14th spot with 4 percent.
- While TB is curable, death can occur when it is diagnosed late.
- The report also highlights a recovery trend in TB diagnosis and treatment services in 2022, signaling a potential reversal of the COVID-19 impact on TB control efforts.
What is Tuberculosis (TB)?
- Tuberculosis (TB) is an infectious disease primarily caused by the bacterium Mycobacterium tuberculosis.
- It mainly affects the lungs but can also impact other parts of the body such as the pleura (lining around the lungs), lymph nodes, intestines, spine, and brain.
- Transmission:
- TB spreads through the air when an infected person with active TB disease coughs, sneezes, or even talks.
- The bacteria can travel through the air and be inhaled by people who are nearby.
- Symptoms:
- Common symptoms include a persistent cough lasting three weeks or more, chest pain, unintentional weight loss, fatigue, and fever.
- The symptoms may develop gradually, making early detection crucial.
- Treatment for TB:
- TB is treated with a course of antibiotics, typically lasting six to nine months.
- It's crucial to complete the full course to ensure the bacteria are completely eradicated and to prevent drug resistance.
- Prevention:
- Prevention involves vaccination with the Bacillus Calmette-Guérin (BCG) vaccine, particularly in regions with high TB prevalence.
- Avoiding close contact with infected individuals helps prevent transmission.
- Drug-resistant TB:
- Drug-resistant TB occurs when the TB bacteria in a person's body don't respond to, or are resistant to, one or more of the primary TB drugs.
- There are two main categories of drug-resistant TB:
- MDR (multidrug-resistant) TB and
- XDR (extensively drug-resistant) TB.
- MDR TB is characterized by bacteria resistant to at least two vital TB drugs, isoniazid and rifampicin. These drugs are among the most effective in treating TB.
- On the other hand, XDR TB takes resistance a step further. In addition to being resistant to isoniazid and rifampicin, XDR TB strains are also resistant to any fluoroquinolone and at least one of three injectable second-line drugs: amikacin, kanamycin, or capreomycin.
- This makes XDR TB more challenging to treat, as it doesn't respond to a broader range of medications commonly used against TB.
- The World Health Organization's END TB Strategy, initiated in 2014, sets a goal to globally eradicate the TB epidemic by 2035.
- The strategy targets a 95% reduction in TB-related deaths compared to 2015, a 90% decrease in TB incidence rates by 2035 compared to 2015, and the ambitious aim of ensuring that no families face catastrophic costs due to TB by the year 2035.
Global Initiatives to Combat Tuberculosis:
- The World Health Organization (WHO), in collaboration with the Global Fund and Stop TB Partnership, has introduced the joint initiative "Find. Treat. All. #EndTB."
- The release of the Global Tuberculosis Report by WHO serves as a crucial tool in assessing and addressing the global TB situation.
Initiative by Government of India to Tackle Tuberculosis:
- National TB Elimination Programme: Prioritizing TB elimination by allocating additional resources under the National Health Mission, intensifying efforts towards achieving the goal of a TB-free India.
- Ayushman Bharat Digital Health Mission: It emphasizes the integration of technology by introducing digital health IDs for TB patients.
- This initiative aims to guarantee the availability of accurate diagnostics and appropriate treatment through digital means.
- Pradhan Mantri TB Mukt Bharat Abhiyan: It's an initiative of the Ministry of Health and Family Welfare (MOHFW) to accelerate the country’s progress towards TB elimination by 2025.
- Ni-kshay Poshan Yojana: It provides Rs 500 support through direct benefit transfer to eligible patients.
- Currently, two vaccines VPM (Vaccine Projekt Management) 1002 and MIP (Mycobacterium Indicus Pranii) have been developed and identified for TB, and are under Phase-3 clinical trial.
Way Forward
- Specialized Active Case Finding Drives: Launch targeted campaigns to actively identify and diagnose TB cases in specific populations.
- Scaling Up of Molecular Diagnostics to Block Levels: Expanding the use of molecular diagnostic techniques to the grassroots level for efficient and accurate TB detection.
- Decentralization of Screening Services through Ayushman Bharat Health & Wellness Centres: Extending screening services to local health and wellness centers under the Ayushman Bharat initiative, making TB detection more accessible.
- Private Sector Engagement: Collaborating with the private sector to enhance TB case identification and treatment.
- Newer Patient-Centric Initiatives: Introducing innovative models like the Family Caregiver Model and Differentiated Care to reduce mortality and improve treatment success rates.
