Passive Euthanasia in India
- 30 Nov 2025
In News:
In a recent case, the Supreme Court directed the District Hospital, Noida, to constitute a Primary Medical Board to examine whether life-sustaining treatment can be withdrawn for a 32-year-old man in a persistent vegetative state (PVS) for over 12 years. The petition, filed by the patient’s father, sought passive euthanasia, not active intervention. The Court, while acknowledging the patient’s irreversible condition and total disability, reaffirmed that any decision must strictly follow the safeguards laid down in its earlier judgments, and sought a medical report within two weeks before taking a final call.
Understanding Euthanasia and Persistent Vegetative State
A Persistent Vegetative State (PVS) is a condition where higher brain functions such as awareness and cognition are irreversibly lost, while basic functions like breathing, circulation and reflexes continue.
Euthanasia refers to intentionally accelerating death to relieve suffering from an incurable condition and is broadly of two types:
- Active Euthanasia: Direct action to end life (illegal in India).
- Passive Euthanasia: Withholding or withdrawing life-sustaining treatment, allowing natural death.
India permits only passive euthanasia, subject to strict legal and procedural safeguards.
Legal Position in India
Indian law does not recognise an unfettered “right to die” under Article 21, but the Supreme Court has interpreted the right to life to include the right to die with dignity in exceptional circumstances.
- Active euthanasia is prohibited and punishable under the Bharatiya Nyaya Sanhita, 2023, as culpable homicide or murder.
- Passive euthanasia is legally permissible under judicially evolved safeguards.
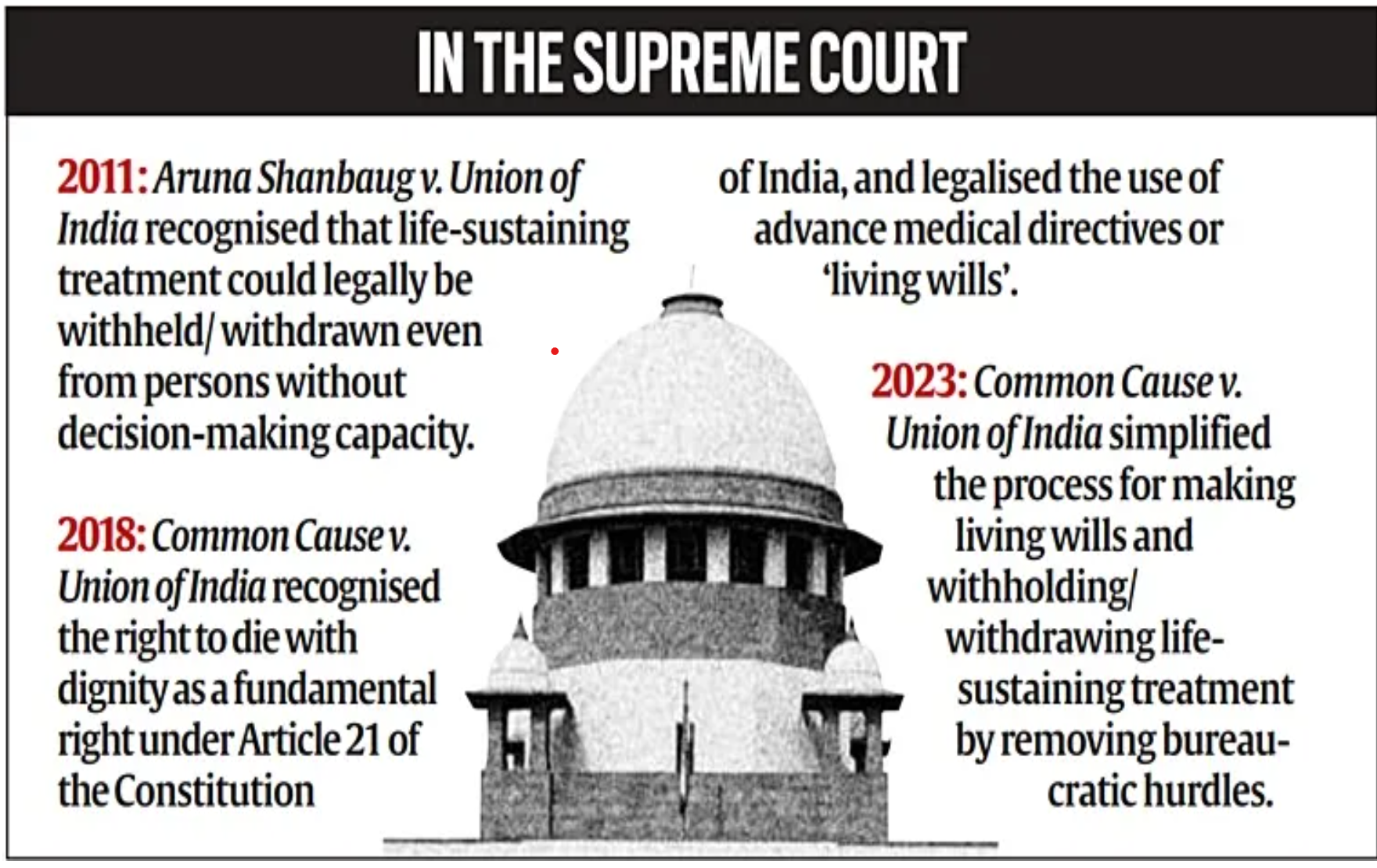
Key judicial milestones include:
- Aruna Shanbaug case (2011): Allowed withdrawal of life support for incompetent patients under court supervision.
- Common Cause case (2018): Recognised passive euthanasia and validated advance medical directives (living wills) for competent adults.
- 2023 modifications: Simplified procedures by reducing medical board size and experience requirements, and setting clear timelines to make the process workable.
Procedural Safeguards
The Supreme Court mandates a two-tier medical review:
- Primary Medical Board constituted by the hospital.
- Secondary Medical Board at the district level.
These boards assess the medical condition, irreversibility, and best interests of the patient. Judicial oversight ensures protection against misuse while respecting dignity.
Ethical Dimensions
The euthanasia debate reflects a tension between competing ethical principles:
- Arguments in favour emphasise autonomy, compassion, minimisation of suffering, and rational allocation of scarce medical resources.
- Arguments against stress the sanctity of life, the doctor’s duty of non-maleficence, risks of a slippery slope, and erosion of trust in medical ethics.
India’s approach attempts a middle path rejecting active killing while permitting dignified death in narrowly defined circumstances.
Global Perspective
Countries such as the Netherlands and Belgium permit both euthanasia and assisted suicide under strict laws, while others like Switzerland allow assisted suicide but prohibit active euthanasia. These variations show that euthanasia is shaped as much by societal values as by medical capability.
Conclusion
The Supreme Court’s direction to constitute a medical board reflects India’s cautious, dignity-centric approach to end-of-life decisions. By balancing compassion with safeguards, autonomy with ethics, and medical judgment with judicial oversight, India seeks to ensure that death, when inevitable, is humane rather than mechanical. As medical technology prolongs biological life, evolving jurisprudence on passive euthanasia will remain crucial to uphold constitutional morality, human dignity and ethical restraint.
Passive Euthanasia for Rabies Patients: SC to Hear Plea
- 16 Feb 2025
In News:
The Supreme Court of India has recently agreed to hear a plea seeking the right to passive euthanasia for rabies patients, citing the exceptional nature of the disease and the absence of a cure. The matter, listed for hearing after two weeks, is poised to test the scope and application of the 2018 passive euthanasia ruling under Article 21 of the Constitution.
Background of the Case
- The petition was filed by the NGO All Creatures Great and Small in 2019, challenging a Delhi High Court order (July 2019) which refused to classify rabies as an exceptional case warranting "death with dignity".
- The Supreme Court issued notice in January 2020 to the Centre and other stakeholders, seeking their response.
- On February 10, 2025, a bench of Justices B.R. Gavai and K. Vinod Chandran agreed to hear the matter after two weeks.
Grounds for the Plea
The NGO has urged the Court to lay down a specific protocol enabling terminally ill rabies patients or their guardians to opt for passive euthanasia under medical supervision. Key arguments include:
- Rabies has a 100% fatality rate once symptoms appear.
- The disease often leads to violent neurological symptoms, requiring patients to be tied or shackled to beds, stripping them of dignity and personal freedom.
- The intense suffering and irreversible nature of rabies, coupled with the lack of any effective treatment, makes it distinct from other terminal conditions.
- The plea seeks the creation of an exceptional legal category for rabies within the framework of the 2018 Supreme Court judgment.
Understanding Euthanasia in India
Definitions:
- Euthanasia literally means “good death” and refers to hastening death to relieve pain and suffering.
- Active Euthanasia involves deliberate acts to cause death (e.g., lethal injection) and remains illegal in India.
- Passive Euthanasia involves withholding or withdrawing life support from terminally ill patients and was legalised in 2018.
Legal Milestone:
- In the Common Cause v. Union of India (2018) case, a five-judge Constitution Bench ruled that the right to die with dignity is a part of the fundamental right to life under Article 21.
- The verdict permitted passive euthanasia and the creation of a “living will”—a legal document allowing patients to refuse life support if in a terminal or vegetative state.
Ethical and Constitutional Dimensions
- The plea raises significant questions about human dignity, bodily autonomy, and the limits of state intervention in end-of-life decisions.
- It also brings focus to judicial responsibility in expanding fundamental rights, especially in the context of terminal, untreatable illnesses.
Conclusion
The outcome of this case could have far-reaching implications on medical jurisprudence and the ethics of end-of-life care in India. If the Court recognizes rabies as an exception, it may set a precedent for disease-specific passive euthanasia protocols, expanding the practical application of the 2018 ruling.
The right to die with dignity
- 26 Oct 2024
In News:
- The Ministry of Health and Family Welfare's draft guidelines (October 2024) aim to implement the Supreme Court's 2018 and 2023 orders on the right to die with dignity.
Legal Context: Supreme Court Rulings and Constitutional Rights
- Right to Refuse Treatment:
- Common Law & Article 21: The right to refuse medical treatment is grounded in common law and is now recognized as a fundamental right under Article 21 of the Indian Constitution, following the 2018 Supreme Court judgment in Common Cause v. Union of India.
- Supreme Court Rulings: The court's rulings in 2018 and 2023 affirmed that individuals have the constitutional right to refuse life-sustaining treatment and to die with dignity.
Withholding and Withdrawing Life-Sustaining Treatment
- Definition and Meaning:
- What Is Life-Sustaining Treatment? Life-sustaining treatments, such as ventilators and feeding tubes, artificially replace vital bodily functions to sustain life.
- Withholding/Withdrawal: This refers to discontinuing these treatments when they no longer improve the patient's condition or merely prolong suffering.
- When Is It Done?
- End-of-Life Care: Withholding or withdrawing treatment is considered when further medical intervention is futile and would only artificially prolong the dying process.
- Focus on Comfort: After withdrawing life-sustaining measures, the focus shifts to palliative care to alleviate pain and suffering.
Understanding Euthanasia and Misconceptions
- What Is Euthanasia?
- Definition: Euthanasia refers to the intentional ending of a terminally ill patient’s life by medical professionals to relieve suffering.
- Passive Euthanasia Misconception: In India, the term "passive euthanasia" is often mistakenly used to describe withholding or withdrawing life-sustaining treatment, but this does not involve the active killing of the patient.
- Legal Framework: The Indian Council of Medical Research (ICMR) clarified in 2018 that "passive euthanasia" is not a legally accepted practice in the country.
The Role of Doctors: Ethical Dilemmas and Shared Decision-Making
- Is Withdrawing Treatment "Giving Up" on the Patient?
- Not Abandonment: Withdrawing life-sustaining treatment is not about abandoning the patient but recognizing when further interventions would cause unnecessary suffering.
- Palliative Care: The patient’s comfort and dignity are prioritized through palliative care, which focuses on pain management and emotional support for both the patient and family.
- Doctors' Ethical Responsibility:
- Shared Decision-Making: The process encourages a collaborative approach between doctors and the patient’s family or surrogate decision-makers. This joint decision-making ensures that the wishes of the patient are respected and relieves the doctor from bearing sole responsibility for life-and-death decisions.
Living Wills and Advance Medical Directives
- What Is a Living Will?
- Definition: A living will is a legal document where a person outlines their medical preferences in the event they lose decision-making capacity.
- Eligibility and Process: Individuals aged 18 or older, who are capable of making decisions, can draft a living will, naming at least two trusted surrogate decision-makers.
- Legal Requirements: The document must be signed in the presence of an executor, two witnesses, and notarized to be legally binding.
- 2023 Supreme Court Guidelines: The Court simplified the procedure for making living wills to ensure that the right to die with dignity is upheld.
Medical Procedure for Withholding or Withdrawing Treatment
- Supreme Court Guidelines
- The Supreme Court laid out a clear procedure for withholding or withdrawing life-sustaining treatment, emphasizing patient autonomy, expert assessments, and family consent.
- Primary and Secondary Medical Boards:
- Primary Medical Board: The treating hospital sets up a Primary Medical Board, consisting of the treating doctor and two subject-matter experts, to assess the patient's condition and determine if life-sustaining treatment is appropriate.
- Secondary Medical Board: A Secondary Medical Board, comprising independent experts, reviews the Primary Board's decision for added oversight.
- Consent from Family/Surrogate Decision-Makers:
- The patient’s wishes, as outlined in an advance directive or by a surrogate, must be respected, and their consent is essential for proceeding with treatment withdrawal.
- Judicial Oversight:
- Once the decision to withdraw treatment is made, the hospital is required to notify the local judicial magistrate, ensuring transparency and accountability.
Conclusion: Legal and Ethical Clarity in End-of-Life Care
- Shared Decision-Making: The process ensures that medical teams, families, and surrogate decision-makers collaborate, preventing any medical professional from facing moral or legal dilemmas alone.
- Protection of Autonomy: These frameworks and guidelines uphold patient autonomy, offering a legal and ethical pathway for terminally ill patients to exercise their right to die with dignity.
